人間のバイオフィールドはラジオ波やマイクロ波の影響を受けているのか?
本記事は、ロバート・O・ヤング博士のScientific Postsの記事を和訳したものです。元記事URLはこちらです:https://www.drrobertyoung.com/post/is-the-human-biofield-negatively-effected-by-radio-microwaves
新型コロナウイルス感染症COVID-19と、5Gを含む無線通信による高周波への曝露との関連性を示すエビデンス!

概要 背景と狙い:
コロナウイルス感染症(COVID-19)の公衆衛生政策は、重症急性呼吸器症候群コロナウイルス2(SARS-CoV-2)ウイルスとその人体への影響に焦点が当てられ、環境要因はほとんど無視されてきた。そこで,COVID-19パンデミックの環境要因として考えられる,マイクロ波やミリ波を含む無線通信システムからの高周波放射について検討した。COVID-19パンデミックの原因ウイルスであるSARS-CoV-2は,中国の武漢で市全体(第5世代[5G]の無線通信放射線[WCR])が導入された直後に表面化し,急速に世界に広がり,当初は,最近5Gネットワークが構築された国際社会と統計的な相関関係を示していた。
※放射(ほうしゃ、英: radiation)は、粒子線(アルファ線、ベータ線など)や電磁波(光など)が放出されること、または放出された粒子線や電磁波そのものをいう。
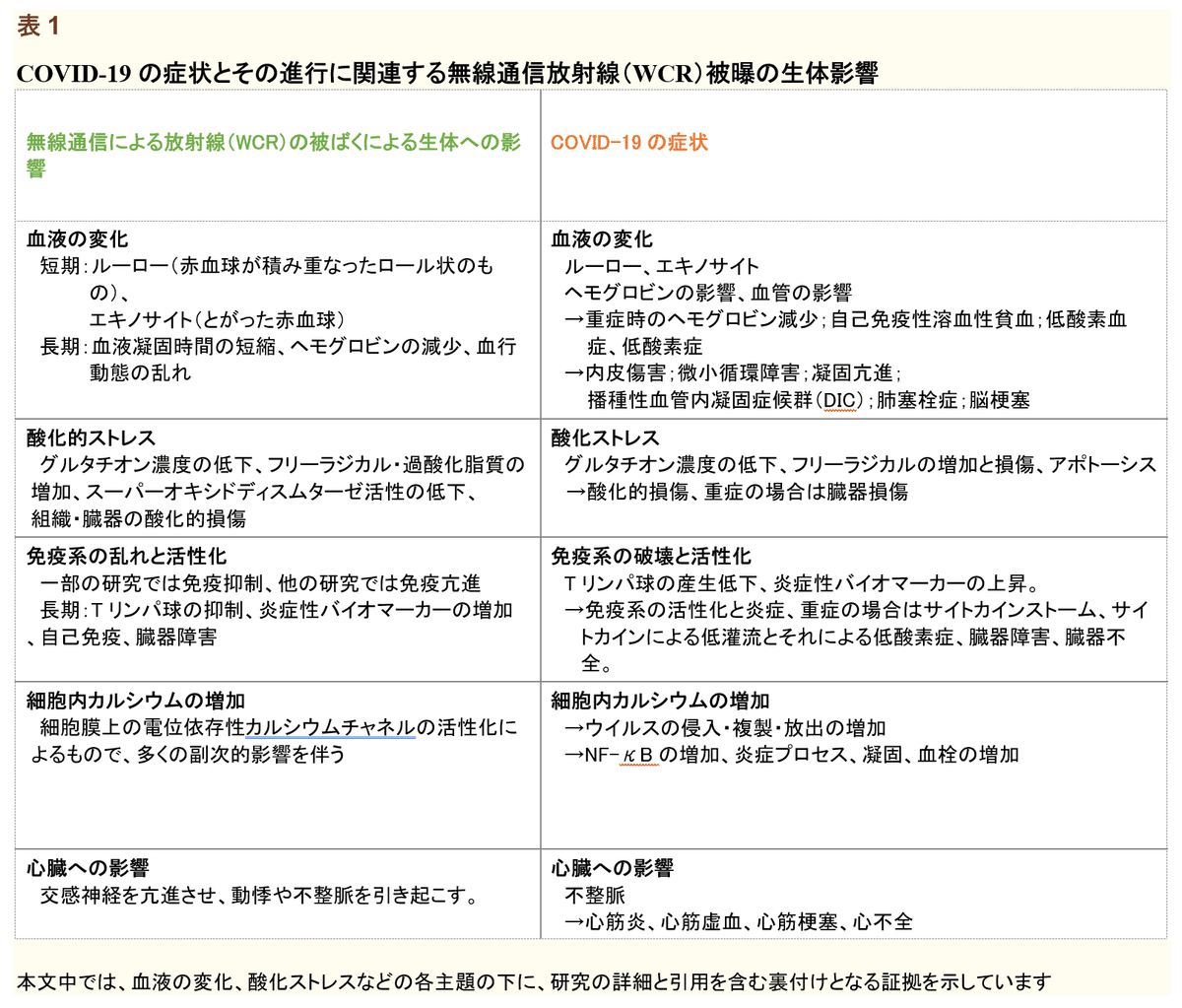
本研究では、WCRの有害な生体影響に関する査読付き科学文献を調査し、WCRが有害な環境因子としてCOVID-19パンデミックに寄与した可能性があるメカニズムをいくつか特定した。生物物理学と病態生理学の分野の垣根を越えて、我々はWCRが以下の可能性を持つという証拠を提示した。(1) エキノサイト(棘状赤血球)やルーロー(連銭)の形成を含む赤血球の形態的変化を引き起こし、凝固亢進の一因となる (2) 微小循環が損なわれ、赤血球やヘモグロビンのレベルが低下し、低酸素症を悪化させる (3) 免疫抑制、自己免疫、炎症亢進などの免疫系の機能障害を増幅させる。(4) 細胞の酸化ストレスやフリーラジカルの生成を増加させ、血管障害や臓器障害を引き起こす。(5) ウイルスの侵入、複製、放出に不可欠な細胞内のCa2+を増加させ、さらに炎症を促進する。(6)不整脈や心疾患を悪化させる。

新型コロナウイルス感染症と5Gを含む無線通信による高周波への曝露との関連性を示す証拠
上記論文の和訳記事
ロバート・O・ヤング博士が研究したヒトの血液細胞への電磁波の影響 - 1998年

VID-19の症状の真の原因は5Gである~ボーダフォンの内部告発者が語る5Gの終焉!
日本語字幕動画
References
[1] Centers for Disease Control and Prevention. Epidemiological Triad. Atlanta, Georgia: Centers for Disease Control and Prevention; 2020. [Google Scholar]
[2] Balmori A. Electromagnetic Pollution from Phone Masts. Effects on Wildlife. Pathophysiology. 2009;16:191–9. [PubMed] [Google Scholar]
[3] Lin JC. 5G Communications Technology and Coronavirus Disease. IEEE Microw Mag. 2020;21:16–9. [Google Scholar]
[4] Mordachev VI. Correlation between the Potential Electromagnetic Pollution Level and the Danger of COVID-19. 4G/5G/6G can be Safe for People. Doklady BGUIR. 2020;18:96–112. [Google Scholar]
[5] Tsiang A, Havas M. COVID-19 Attributed Cases and Deaths are Statistically Higher in States and Counties with 5th Generation Millimeter Wave Wireless Telecommunications in the United States. Med Res Arch. 2021;9:2371. [Google Scholar]
[6] Ing AJ, Cocks C, Green JP. COVID-19:In the Footsteps of Ernest Shackleton. Thorax. 2020;75:693–4. [PMC free article] [PubMed] [Google Scholar]
[7] Garg S, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 COVID-NET 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 69:458–64. [PMC free article] [PubMed] [Google Scholar]
[8] Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease. JAMA Intern Med. 2020;180:934–43. [PMC free article] [PubMed] [Google Scholar]
[9] Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 Pneumonia:Different Respiratory Treatments for Different Phenotypes. Intensive Care Med. 2020;46:1099–102. [PMC free article] [PubMed] [Google Scholar]
[10] Cecchini R, Cecchini AL. SARS-CoV-2 Infection Pathogenesis is Related to Oxidative Stress as a Response to Aggression. Med Hypotheses. 2020;143:110102. [PMC free article] [PubMed] [Google Scholar]
[11] Cavezzi A, Troiani E, Corrao S. COVID-19:Hemoglobin, Iron, and Hypoxia Beyond Inflammation, a Narrative Review. Clin Pract. 2020;10:1271. [PMC free article] [PubMed] [Google Scholar]
[12] Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, et al. Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease:Implications for Prevention, Antithrombotic Therapy, and Follow-Up:JACC State-of-the-Art Review. JACC. 2020;75:2950–73. [PMC free article] [PubMed] [Google Scholar]
[13] Carfi A, Bernabei R, Landi F. Persistent Symptoms in Patients after Acute COVID-19. JAMA. 2020;324:603–5. [PMC free article] [PubMed] [Google Scholar]
[14] CNIRP. International Commission on Non-Ionizing Radiation Protection (ICNIRP) Guidelines for
Limiting Exposure to Electromagnetic Fields (100 kHz to 300 GHz) Health Phys. 2020;118:483–524. [PubMed] [Google Scholar]
[15] Bortkiewicz A, Gadzicka E, Szymczak W. Mobile Phone Use and Risk for Intracranial Tumors and Salivary Gland Tumors A Meta-analysis. Int J Occup Med Environ Health. 2017;30:27–43. [PubMed] [Google Scholar]
[16] Sangün Ö, Dündar B, Çömlekçi S, Büyükgebiz A. The Effects of Electromagnetic Field on the Endocrine System in Children and Adolescents. Pediatr Endocrinol Rev. 2016;13:531–45. [PubMed] [Google Scholar]
[17] Yakymenko I, Tsybulin O, Sidorik E, Henshel D, Kyrylenko O, Kyrylenko S. Oxidative Mechanisms of Biological Activity of Low-intensity Radiofrequency Radiation. Electromagn Biol Med. 2016;35:186–202. [PubMed] [Google Scholar]
[18] Ruediger HW. Genotoxic Effects of Radiofrequency Electromagnetic Fields. Pathophysiology. 2009;16:89–102. [PubMed] [Google Scholar]
[19] Asghari A, Khaki AA, Rajabzadeh A, Khaki A. A Review on Electromagnetic Fields (EMFs) and the Reproductive System. Electron Physician. 2016;8:2655–62. [PMC free article] [PubMed] [Google Scholar]
[20] Zhang J, Sumich A, Wang GY. Acute Effects of Radiofrequency Electromagnetic Field Emitted by Mobile Phone on Brain Function. Bioelectromagnetics. 2017;38:329–38. [PubMed] [Google Scholar]
[21] Pall ML. Microwave Frequency Electromagnetic Fields (EMFs) Produce Widespread Neuropsychiatric Effects Including Depression. J Chem Neuroanat. 2016;75:43–51. [PubMed] [Google Scholar]
[22] Avendano C, Mata A, Sanchez Sarmiento CA, Doncei GF. Use of Laptop Computers Connected to Internet through Wi-Fi Decreases Human Sperm Motility and Increases Sperm DNA Fragmentation. Fertil Steril. 2012;97:39–45. [PubMed] [Google Scholar]
[23] Buchner K, Eger H. Changes of Clinically Important Neurotransmitters under the Influence of Modulated RF Fields a Long-term Study Under Real-life Conditions Umwelt Medizin Gesellschaft. 2011;24:44–57. [Google Scholar]
[24] Navarro EA, Segura J, Portoles M, Gomez-Perretta C. The Microwave Syndrome:A Preliminary Study in Spain. Electromagn Biol Med. 2003;22:161–9. [Google Scholar]
[25] Hutter HP, Moshammer H, Wallner P, Kundi M. Subjective Symptoms, Sleeping Problems, and Cognitive Performance in Subjects Living Near Mobile Phone Base Stations. Occup Environ Med. 2006;63:307–13. [PMC free article] [PubMed] [Google Scholar]
[26] Magras IN, Xenos TD. RF Radiation-induced Changes in the Prenatal Development of Mice. Bioelectromagnetics. 1997;18:455–61. [PubMed] [Google Scholar]
[27] Glaser ZR. Project MF12.524.015-00043 Report No. 2. Bethesda, MD: Naval Medical Research Institute; 1972. Bibliography of Reported Biological Phenomena ('Effects') and Clinical Manifestations Attributed to Microwave and Radio-Frequency Radiation Research Report; pp. 1–103. [Google Scholar]
[28] Glaser ZR, Brown PF, Brown MS. Bibliography of Reported Biological Phenomena (Effects) and Clinical Manifestations Attributed to Microwave and Radio-Frequency Radiation:Compilation and Integration of Report and Seven Supplements. Bethesda, MD:Naval Medical Research Institute. 1976:1–178. [Google Scholar]
[29] Belyaev IY, Shcheglov VS, Alipov YD, Polunin VA. Resonance Effect of Millimeter Waves in the Power Range from 10(-19) to 3 x 10(-3) W/cm2 on Escherichia coli Cells at Different Concentrations. Bioelectromagnetics. 1996;17:312–21. [PubMed] [Google Scholar]
[30] Grigoriev YG, Grigoriev OA, Ivanov AA, Lyaginskaya AM, Merkulov AV, Shagina NB, et al. Confirmation Studies of Soviet Research on Immunological Effects of Microwaves:Russian Immunology Results. Bioelectromagnetics. 2010;31:589–602. [PubMed] [Google Scholar]
[31] Grigoriev Y. Mobile Communications and Health of Population:The Risk Assessment, Social and Ethical Problems. Environmentalist. 2012;32:193–200. [Google Scholar]
[32] Repacholi M, Grigoriev Y, Buschmann J, Pioli C. Scientific Basis for the Soviet and Russian Radiofrequency Standards for the General Public. Bioelectromagnetics. 2012;33:623–33. [PubMed] [Google Scholar]
[33] Pakhomov A, Murphy M. A Comprehensive Review of the Research on Biological Effects of Pulsed Radiofrequency Radiation in Russia and the Former Soviet Union. 2011 [Google Scholar]
[34] Belyaev IY. Dependence of Non-thermal Biological Effects of Microwaves on Physical and Biological Variables:Implications for Reproducibility and Safety Standards. Eur J Oncol. 2010;5:187–218. [Google Scholar]
[35] Franzen J. Wideband Pulse Propagation in Linear Dispersive Bio-Dielectrics Using Fourier Transforms. United States Air Force Research Laboratory Report No. AFRL-HE-BR-TR-1999-0149. 1999 February; [Google Scholar]
[36] Albanese R, Penn J, Medina R. Short-rise-time Microwave Pulse Propagation through Dispersive
Biological Media. J Opt Soc Am A. 1989;6:1441–6. [Google Scholar]
[37] Lin-Liu S, Adey WR. Low Frequency Amplitude Modulated Microwave Fields Change Calcium Efflux Rates from Synaptosomes. Bioelectromagnetics. 1982;3:309–22. [PubMed] [Google Scholar]
[38] Penafiel LM, Litovitz T, Krause D, Desta A, Mullins MJ. Role of Modulation on the Effect of Microwaves on Ornithine Decarboxylase Activity in L929 Cells. Bioelectromagnetics. 1997;18:132–41. [PubMed] [Google Scholar]
[39] Huber R, Treyer V, Borbely AA, Schuderer J, Gottselig JM, Landolt HP, Werth E, et al. Electromagnetic Fields, Such as Those from Mobile Phones, Alter Regional Cerebral Blood Flow and Sleep and Waking EEG. J Sleep Res. 2002;11:289–95. [PubMed] [Google Scholar]
[40] Panagopoulos DJ, Karabarbounis A, Margaritis LH. Mechanism of Action of Electromagnetic Fields on Cells. Biochem Biophys Res Commun. 2002;298:95–102. [PubMed] [Google Scholar]
[41] Panagopoulos DJ. Comments on Pall's Millimeter (MM) Wave and Microwave Frequency Radiation Produce Deeply Penetrating Effects:The Biology and the Physics. Rev Environ Health. 2021;2021:165. [PubMed] [Google Scholar]
[42] Sage C, Carpenter DO. BioInitiative Working Group. BioInitiative Report:A Rationale for a Biologically-based Public Exposure Standard for Electromagnetic Radiation. Updated 2014-2020. 2012. http://www.bioinitiative.org.
[43] Belpomme D, Hardell L, Belyaev I, Burgio E, Carpenter DO. Thermal and Non-thermal Health Effects of Low Intensity Non-ionizing Radiation:An International Perspective (Review) Environ Pollut. 2018;242:643–58. [PubMed] [Google Scholar]
[44] Di Ciaula A. Towards 5G Communication Systems:Are there Health Implications? Int J Hyg Environ Health. 2018;221:367–75. [PubMed] [Google Scholar]
[45] Russell CL. 5G Wireless Telecommunications Expansion:Public Health and Environmental Implications. Environ Res. 2018;165:484–95. [PubMed] [Google Scholar]
[46] Miller AB, Sears ME, Morgan LL, Davis DL, Hardell L, Oremus M, et al. Risks to Health and Well-being from Radio-frequency Radiation Emitted by Cell Phones and Other Wireless Devices. Public Health Front. 2019;7:223. [PMC free article] [PubMed] [Google Scholar]
[47] Pakhomov AG, Akyel Y, Pakhomova ON, Stuck BE, Murphy MR. Current State and Implications of Research on the Biological Effects of Millimeter Waves. Bioelectromagnetics. 1998;19:393–413. [PubMed] [Google Scholar]
[48] Betskii OV, Lebedeva NN. In:Clinical Application of Bioelectromagnetic Medicine. New York: Marcel Decker; 2004. Low-intensity Millimeter Waves in Biology and Medicine; pp. 30–61. [Google Scholar]
[49] Kostoff RN, Block JA, Solka JL, Briggs MB, Rushenberg RL, Stump JA, et al. Literature-Related Discovery:A Review. Report to the Office of Naval Research. 2007:1–58. [Google Scholar]
[50] Havas M. Radiation from Wireless Technology Affects the Blood, Heart, and the Autonomic Nervous System. Rev Environ Health. 2013;28:75–84. [PubMed] [Google Scholar]
[51] Rubik B. Does Short-term Exposure to Cell Phone Radiation Affect the Blood? Wise Trad Food Farm Heal Arts. 2014;15:19–28. [Google Scholar]
[52] Wagner C, Steffen P, Svetina S. Aggregation of Red Blood Cells:From Rouleaux to Clot Formation. Comput Rendus Phys. 2013;14:459–69. [Google Scholar]
[53] Lakhdari N, Tabet B, Boudraham L, Laoussati M, Aissanou S, Beddou L, et al. Red Blood Cells Injuries and Hypersegmented Neutrophils in COVID-19 Peripheral. medRxiv. 2020;2020:20160101. [Google Scholar]
[54] Lei Y, Zhang J, Schiavon CR, He M, Chen L, Shen H, et al. SARS-CoV-2 Spike Protein Impairs Endothelial Function Via Downregulation of ACE2. Circ Res. 2021;128:1323–6. [PMC free article] [PubMed] [Google Scholar]
[55] Zhang S, Liu Y, Wang X, Yang L, Li H, Wang Y, et al. SARS-CoV-2 Binds Platelet ACE2 to Enhance Thrombosis in COVID-19. J Hematol Oncol. 2020;13:120. [PMC free article] [PubMed] [Google Scholar]
[56] Zalyubovskaya NP. Biological Effect of Millimeter Radiowaves. Vrachebnoye Delo. 1977;3:116–9. [PubMed] [Google Scholar]
[57] Zalyubovskaya NP, Kiselev RI. Effects of Radio Waves of a Millimeter Frequency Range on the Body of Man and Animals. Gigiyna I Sanitaria. 1978;8:35–9. [Google Scholar]
[58] Wenzhong L, Li H. COVID-19 Attacks the 1-beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Heme Metabolism. ChemRxiv. 2020;2020:26434. [Google Scholar]
[59] Lippi G, Mattiuzzi C. Hemoglobin Value May be Decreased in Patients with Severe Coronavirus Disease 2019. Hematol Transfus Cell Ther. 2020;42:116–7. [PMC free article] [PubMed] [Google Scholar]
[60] Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 Expression in Human Heart Indicates New Potential Mechanism of Heart Injury among Patients Infected with SARS-CoV-2. Cardiovasc Res. 2020;116:1097–100. [PMC free article] [PubMed] [Google Scholar]
[61] Algassim, AA, Elghazaly AA, Alnahdi AS, Mohammed-Rahim OM, Alanazi AG, Aldhuwayhi NA, et al. Prognostic Significance of Hemoglobin Level and Autoimmune Hemolytic Anemia in SARS-CoV-2 Infection. Ann Hematol. 2021;100:37–43. [PMC free article] [PubMed] [Google Scholar]
[62] Ghahramani S, Tabrizi R, Lankarani KB, Kashani SMA, Rezaei S, Zeidi N, et al. Laboratory Features of Severe vs Non-severe COVID-19 Patients in Asian Populations:A Systematic Review and Meta-analysis. Eur J Med Res. 2020;25:30. [PMC free article] [PubMed] [Google Scholar]
[63] Cheng L, Li HL, Li C, Liu C, Yan S, Chen H, et al. Ferritin in the Coronavirus Disease 2019 (COVIDvirus A Systematic Review and Meta?etaemati. J Clin Lab Anal. 2020;34:e23618. [PMC free article] [PubMed] [Google Scholar]
[64] Tobin MJ, Laghi F, Jubran A. Why COVID-19 Silent Hypoxemia is Baffling to Physicians. Am J Respir. 2020;202:356–60. [PMC free article] [PubMed] [Google Scholar]
[65] Ejigu T, Patel N, Sharma A, Vanjarapu JMR, Nookala V. Packed Red Blood Cell Transfusion as a Potential Treatment Option in COVID-19 Patients with Hypoxemic Respiratory Failure:A Case Report. Cureus. 2020;12:e8398. [PMC free article] [PubMed] [Google Scholar]
[66] Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial Cell Infection and Endotheliitis in COVID-19. Lancet. 2020;395:1417–8. [PMC free article] [PubMed] [Google Scholar]
[67] Betteridge DJ. What is Oxidative Stress? Metabolism. 2000;49(2 Suppl 1):3–8. [PubMed] [Google Scholar]
[68] Giamarellos-Bourboulis E, Netea MG, Rovina N, Akinosoglou K, Antoniadou A, Antonakos N, et al. Complex Immune Dysregulation in COVID-19 Patients with Severe Respiratory Failure. Cell Host Microbe. 2020;27:992–1000. [PMC free article] [PubMed] [Google Scholar]
[69] Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, et al. Impaired Type 1 Interferon Activity and Inflammatory Responses in Severe COVID-19 Patents. Science. 2020;369:718–24. [PMC free article] [PubMed] [Google Scholar]
[70] Dasdag S, Akdag MZ. The Link between Radiofrequencies Emitted from Wireless Technologies and Oxidative Stress. J Chem Neuroanat. 2016;75:85–93. [PubMed] [Google Scholar]
[71] Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial Function and Oxidative Stress in Cardiovascular Diseases. Circ J. 2009;73:411–8. [PubMed] [Google Scholar]
[72] Polonikov A. Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Manifestations and Death in COVID-19 Patients. ACS Infect Dis. 2020;6:1558–62. [PMC free article] [PubMed] [Google Scholar]
[73] Guloyan V, Oganesian B, Baghdasaryan N, Yeh C, Singh M, Guilford F, et al. Glutathione Supplementation as an Adjunctive Therapy in COVID-19. Antioxidants (Basel, Switzerland) 2020;9:914. [PMC free article] [PubMed] [Google Scholar]
[74] Marushchak M, Maksiv K, Krynytska I, Dutchak O, Behosh N. The Severity of Oxidative Stress in Comorbid Chronic Obstructive Pulmonary Disease (COPD) and Hypertension:Does it Depend on ACE and AGT Gene Polymorphisms? J Med Life. 2019;12:426–34. [PMC free article] [PubMed] [Google Scholar]
[75] Choromanska B, Mysiliwiec P, Luba M, Wojskowicz P, Mysliwiec H, Choromanska K, et al. The Impact of Hypertension and Metabolic Syndrome on Nitrosative Stress and Glutathione Metabolism in Patients with Morbid Obesity. Oxid Med Cell Longev. 2020;2020:1057570. [PMC free article] [PubMed] [Google Scholar]
[76] Lutchmansingh FK, Hsu JW, Bennett FI, Badaloo AV, Mcfarlane-Anderson N, Gordon-Strachan GM, et al. Glutathione Metabolism in Type 2 Diabetes and its Relationship with Microvascular Complications and Glycemia. PLoS One. 2018;13:e0198626. [PMC free article] [PubMed] [Google Scholar]
[77] Horowitz RI, Freeman PR, Bruzzese J. Efficacy of Glutathione Therapy in Relieving Dyspnea Associated with COVID-19 Pneumonia:A Report of 2 Cases. Respir Med. 2020;30:101063. [PMC free article] [PubMed] [Google Scholar]
[78] Peraica M, Marijanovic AM, Flajs D, Domijan AM, Gajski G, Garaj-Vrhovac G. Oxidative Stress in Workers Occupationally Exposed to Microwave Radiation. Toxicol Lett. 2008;180:38–9. [Google Scholar]
[79] Garaj-Vrhovac V, Gajski G, Pazanin S, Sarolic A, Domijan D, Flajs D, et al. Assessment of Cytogenetic Damage and Oxidative Stress in Personnel Occupationally Exposed to the Pulsed Microwave Radiation of Marine Radar Equipment. Int J Hyg Environ Health. 2011;214:59–65. [PubMed] [Google Scholar]
[80] Zothansiama Zosangzuali M, Lalramdinpuii M, Jagetia GC. Impact of Radiofrequency Radiation on DNA Damage and Antioxidants in Peripheral Blood Lymphocytes of Humans Residing in the Vicinity of Mobile Phone Base Stations. Electromagn Biol Med. 2017;36:295–305. [PubMed] [Google Scholar]
[81] Moustafa YM, Moustafa RM, Belacy A, Abou-El-Ela SH, Ali FM. Effects of Acute Exposure to the Radiofrequency Fields of Cellular Phones on Plasma Lipid Peroxide and Anti-oxidase Activities in Human Erythrocytes. J Pharm Biomed Anal. 2001;26:605–8. [PubMed] [Google Scholar]
[82] Hassan NS, Rafaat BM, Aziz SW. Modulatory Role of Grape Seed Extract on Erythrocyte Hemolysis and Oxidative Stress Induced by Microwave Radiation in Rats. Int J Integr Biol. 2010;10:106–11. [Google Scholar]
[83] Yurekli AI, Ozkan M, Kalkan T, Saybasili H, Tuncel H, Atukeren P, et al. GSM Base Station Electromagnetic Radiation and Oxidative Stress in Rats. Electromagn Biol Med. 2006;25:177–88. [PubMed] [Google Scholar]
[84] Dasdag S, Bilgin HM, Akdag MZ, Celik H, Aksen F. Effect of Long-term Mobile Phone Exposure on Oxidative-antioxidative Processes and Nitric Oxide in Rats. Biotechnol Biotechnol Equip. 2008;22:992–7. [Google Scholar]
[85] Alkis ME, Akdag MZ, Dasdag S. Effects of low?intensity Microwave Radiation on Oxidant?antioxidant Parameters and DNA Damage in the Liver of rats. Bioelectromagnetics. 2021;42:76–85. [PubMed] [Google Scholar]
[86] Loscalzo J. Oxidant Stress:A Key Determinant of Atherothrombosis. Biochem Soc Trans. 2003;31:1059–61. [PubMed] [Google Scholar]
[87] Tang N, Li D, Wang X, Sun Z. Abnormal Coagulation Parameters are Associated with Poor Prognosis in Patients with Novel Coronavirus Pneumonia. J Thromb Haemost. 2020;18:844–7. [PMC free article] [PubMed] [Google Scholar]
[88] Klok FA, Kruip MJ, Van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Incidence of Thrombotic Complications in Critically ill ICU Patients with COVID-19. Thromb Res. 2020;191:145–7. [PMC free article] [PubMed] [Google Scholar]
[89] Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and Multi-Organ Response. Curr Probl Cardiol. 2020;2020:100618. [PMC free article] [PubMed] [Google Scholar]
[90] Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS-CoV-2 and Stroke in a New York Healthcare System. Stroke. 2020;51:2002–11. [PMC free article] [PubMed] [Google Scholar]
[91] Bandara P, Weller S. Cardiovascular Disease:Time to Identify Emerging Environmental Risk Factors. Eur J Prev Cardiol. 2017;24:1819–23. [PubMed] [Google Scholar]
[92] Esmekaya MA, Ozer C, Seyhan N. 900 MHz Pulse-modulated Radiofrequency Radiation Induces Oxidative Stress on Heart, Lung, Testis, and Liver Tissues. Gen Physiol Biophys. 2011;30:84–9. [PubMed] [Google Scholar]
[93] Cao X. COVID-19:Immunopathology and its Implications for Therapy. Nat Rev Immunol. 2020;20:269–70. [PMC free article] [PubMed] [Google Scholar]
[94] Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020;71:762–8. [PMC free article] [PubMed] [Google Scholar]
[95] McRee DI. Soviet and Eastern European Research on Biological Effects of Microwave Radiation. Proc IEEE. 1980;68:84–91. [Google Scholar]
[96] Baranski S. Effect of Chronic Microwave Irradiation on the Blood Forming System of Guinea Pigs and Rabbits. Aerosp Med. 1971;42:1196–9. [PubMed] [Google Scholar]
[97] Nageswari KS, Sarma KR, Rajvanshi VS, Sharan R, Sharma M, Barathwal V, et al. Effect of Chronic Microwave Radiation on T Cell-mediated Immunity in the Rabbit. Int. 1991;35:92–7. [PubMed] [Google Scholar]
[98] Adang D, Remacle C, Vander Vorst A. Results of a Long-term Low-level Microwave Exposure of Rats. IEEE Trans Microw Theory Tech. 2009;57:2488–97. [Google Scholar]
[99] McRee DI, Faith R, McConnell EE, Guy AW. Long-term 2450-MHz cw Microwave Irradiation of Rabbits:Evaluation of Hematological and Immunological Effects. J Microw Power Electromagn Energy. 1980;15:45–52. [Google Scholar]
[100] Johansson O. Disturbance of the Immune System by Electromagnetic Fields a Potentially Underlying Cause for Cellular Damage and Tissue Repair Reduction which Could Lead to Disease and Impairment. Pathophysiology. 2009;16:157–77. [PubMed] [Google Scholar]
[101] Szmigielski S. Reaction of the Immune System to Low-level RF/MW Exposures. Sci Total Environ. 2013;454-455:393–400. [PubMed] [Google Scholar]
[102] Zhou F, Ting Y, Du R, Fan G, Liu Y, Liu Z, et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China:A Retrospective Cohort Study. Lancet. 2020;395:1054–62. [PMC free article] [PubMed] [Google Scholar]
[103] Yang M. Cell Pyroptosis, a Potential Pathogenic Mechanism of 2019-nCoV Infection. ScienceOpen. 2020 [Google Scholar]
[104] Upadhyay J, Tiwari N, Ansari MN. Role of Inflammatory Markers in Corona Virus Disease (COVID-19) Patients:A Review. Exp Biol Med. 2020;245:1368–75. [PMC free article] [PubMed] [Google Scholar]
[105] Shandala MG, Rudnev MI, Vinogradov GK, Belonoshko NC, Goncharova NM. Immunological and hematological effects of microwaves at low power densities. In:Proceedings of International Union of Radio Science Symposium on Biological Effects of Electromagnetic Waves. 84 Airlie, VA;1977. [Google Scholar]
[106] Grigoriev YG, Ivanov AA, Lyaginskaya AM, Merkulov AV, Stepanov VS, Shagina NB. Autoimmune Processes after Long-term Low-level Exposure to Electromagnetic Fields (Experimental Results) Part I. Mobile Communications and Changes in Electromagnetic Conditions for the Population. Need for Additional Substantiation of Existing Hygienic Standards. Biophysics. 2010:551041–5. [PubMed] [Google Scholar]
[107] Grigoriev YG. Evidence for Effects on the Immune System. Immune System and EMF RF. Bioinitiative Rep. 2012;8:1–24. [Google Scholar]
[108] Szabo I, Rojavin MA, Rogers, TJ, Ziskin MC. Reactions of Keratinocytes to In Vitro Millimeter Wave Exposure. Bioelectromagnetics. 2001;22:358–64. [PubMed] [Google Scholar]
[109] Makar V, Logani M, Szabo I, Ziskin M. Effect of Millimeter Waves on Cyclophosphamide Induced Suppression of T Cell Functions. Bioelectromagnetics. 2003;24:356–65. [PubMed] [Google Scholar]
[110] Walleczek J. Electromagnetic Field Effects on Cells of the Immune System:The Role of Calcium Signaling. FASEB J. 1992;6:3177–85. [PubMed] [Google Scholar]
[111] Panagopoulos DJ, Messini N, Karabarbounis A, Filippetis AL, Margaritis LH. A Mechanism for Action of Oscillating Electric Fields on Cells. Biochem Biophys Res Commun. 2000;272:634–40. [PubMed] [Google Scholar]
[112] Pall ML. Electromagnetic Fields Act Via Activation of Voltage-gated Calcium Channels to Produce Beneficial or Adverse Effects. J Cell Mol Med. 2013;17:958–65. [PMC free article] [PubMed] [Google Scholar]
[113] Chen X, Cao R, Zhong W. Host Calcium Channels and Pumps in Viral Infections. Cells. 2019;9:94. [PMC free article] [PubMed] [Google Scholar]
[114] Solaimanzadeh I. Nifedipine and Amlodipine are Associated with Improved Mortality and Decreased Risk for Intubation and Mechanical Ventilation in Elderly Patients Hospitalized for COVID-19. Cureus. 2020;12:e8069. [PMC free article] [PubMed] [Google Scholar]
[115] Straus MR, Bidon M, Tang T, Whittaker GR, Daniel S. FDA Approved Calcium Channel Blockers Inhibit SARS-CoV-2 Infectivity in Epithelial Lung Cells. BioRxiv. 2020;2020:214577. [Google Scholar]
[116] Sen CK, Roy S, Packer L. Involvement of Intracellular Ca2+ in Oxidant-Induced NF-κB Activation. FEBS Lett. 1996;385:58–62. [PubMed] [Google Scholar]
[117] Do LA, Anderson J, Mulholland EK, Licciardi PV. Can Data from Paediatric Cohorts Solve the COVID-19 Puzzle? PLoS Pathog. 2020;16:e1008798. [PMC free article] [PubMed] [Google Scholar]
[118] Atri D, Siddiqi HK, Lang JP, Nauffal V, Morrow DA, Bohula EA. COVID-19 for the Cardiologist:Basic Virology, Epidemiology, Cardiac Manifestations, and Potential Therapeutic Strategies. JACC Back Transl Sci. 2020;5:518–36. [PMC free article] [PubMed] [Google Scholar]
[119] Dherange P, Lang J, Qian P, Oberfeld B, Sauer WH, Koplan B, et al. Arrhythmias and COVID-19:A Review. JACC Clin Electrophysiol. 2020;6:1193–204. [PMC free article] [PubMed] [Google Scholar]
[120] Colon CM, Barrios JG, Chiles JW, McElwee SK, Russell DW, Maddox WR, et al. Atrial Arrhythmias in COVID-19 Patients. JACC Clin Electrophysiol. 2020;6:1189–90. [PMC free article] [PubMed] [Google Scholar]
[121] Gökmen N, Erdem S, Toker KA, Ocmen E, Ozkure A. Analyzing Exposures to Electromagnetic Fields in an Intensive Care Unit. Turk J Anaesthesiol Reanim. 2016;44:236–40. [PMC free article] [PubMed] [Google Scholar]
[122] Sandoval Y, Januzzi JL, Jaffe AS. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19. J Am Coll Cardiol. 2020;76:1244–58. [PMC free article] [PubMed] [Google Scholar]
[123] Dodge CH. Clinical and Hygienic Aspects of Exposure to Electromagnetic Fields. Biological Effects and Health Implications of Microwave Radiation. A Review of the Soviet and Eastern European Literature. In:Symposium Proceedings, Richmond, VA. 1969 Sep 17. [Google Scholar]
[124] Jauchem JR. Exposure to Extremely Low Frequency Electromagnetic Fields and Radiofrequency Radiation:Cardiovascular Effects in Humans. Int Arch Occup Environ Health. 1997;70:9–21. [PubMed] [Google Scholar]
[125] Black DR, Heynick LN. Radiofrequency Effects on Blood Cells Cardiac, Endocrine, and Immunological Functions. Bioelectromagnetics. 2003;6:S187–95. [PubMed] [Google Scholar]
[126] Havas M, Marrongelle J, Pollner B, Kelley E, Rees CRG, Tully L. Provocation Study Using Heart Rate Variability Shows Microwave Radiation from 2.4GHz Cordless Phone Affects Autonomic Nervous System. Eur J Oncol Library. 2010;5:271–98. [Google Scholar]
[127] Saili L, Hanini A, Smirani C, Azzouz I, Sakly M, Abdelmelek H, et al. Effects of Acute Exposure to WIFI Signals (2.45GHz) on Heart Variability and Blood Pressure in Albino Rabbits. Environ Toxicol Pharmacol. 2015;40:600–5. [PubMed] [Google Scholar]
[128] Cleary SF. Biological Effects and Health Implications of Microwave Radiation. A Review of the Soviet and Eastern European Literature. In:Symposium Proceedings, Richmond, VA 1969 Sep 17. BRH/DBE Report No. 70-2. 1970 [Google Scholar]
[129] Fiasca F, Minelli M, Maio D, Minelli M, Vergallo I, Necozione S, et al. Associations between
COVID-19 Incidence Rates and the Exposure to PM2.5 and NO2:A Nationwide Observational Study in Italy. Int J Environ Res Public Health. 2020;17:9318. [PMC free article] [PubMed] [Google Scholar]
[130] Hoyt JR, Langwig KE, Sun K, Parise KL, Li A, Wang Y, et al. Environmental Reservoir Dynamics Predict Global Infection Patterns and Population Impacts for the Fungal Disease White-nose Syndrome. PNAS. 2020;117:7255–62. [PMC free article] [PubMed] [Google Scholar]
[131] Federal Communications Commission (FCC). Guidelines for Evaluating the Environmental Effects of Radiofrequency Radiation. FCC96-326;ET Docket No. 93-62. 1996 [Google Scholar]
[132] Belyaev I, Dean A, Eger H, Hubmann G, Jandrisovits R, Kern M, et al. EUROPAEM EMF Guideline 2016 for the Prevention, Diagnosis and Treatment of EMF-related Health Problems and Illnesses. Rev Environ Health. 2016;31:363–97. [PubMed] [Google Scholar]
[133] Huss A, Egger M, Hug K, Huwiler-Muntener K, Roosli M. Source of Funding and Results of Studies of Health Effects of Mobile Phone Use:Systematic Review of Experimental Studies. Environ Health Perspect. 2007;115:14. [PMC free article] [PubMed] [Google Scholar]
[134] Panagopoulos DJ. Comparing DNA Damage Induced by Mobile Telephony and Other Types of Man-made Electromagnetic Fields. Mutat Res. 2019;781:53–62. [PubMed] [Google Scholar]
[135] Belyaev IY, Shcheglov VS, Alipov ED, Ushalov VD. Nonthermal Effects of Extremely High-frequency Microwaves on Chromatin Conformation in cells In Vitro Dependence on Physical, Physiological, and Genetic Factors. IEEE Trans Microw Theory Techn. 2000;48:2172–9. [Google Scholar]
[136] Blackman CF, Kinney LS, Houyse DE, Joines WT. Multiple Power-density Windows and their Possible Origin. Bioelectromagnetics. 1989;10:115–28. [PubMed] [Google Scholar]
[137] Panagopoulos DJ, Cammaerts MC, Favre D, Balmori A. Comments on Environmental Impact of Radiofrequency Fields from Mobile Phone Base Stations. Crit Rev Environ Sci Technol. 2016;46:885–903. [Google Scholar]
[138] Kriebel D, Tickne J, Epstein P, Lemons PJ, Levins R, Loechler EL, et al. The Precautionary Principle in Environmental Science. Environ Health Perspect. 2001;109:871–6. [PMC free article] [PubMed] [Google Scholar]
[139] Tretyakov MY, Koshelev MA, Dorovskikh VV, Makarov DS, Rosenkranz PW. 60-GHz Oxygen Band:Precise Broadening and Central Frequencies of Fine-Structure Lines, Absolute Absorption Profile at Atmospheric Pressure, and Revision of Mixing Coefficients. J Mol Spectrosc. 2005;231:1–14. [Google Scholar]
[140] Torgomyan H, Kalantaryan V, Trchounian A. Low Intensity Electromagnetic Irradiation with 70.6 and 73 GHz Frequencies Affects Escherichia coli Growth and Changes Water Properties. Cell Biochem Biophys. 2011;60:275–81. [PubMed] [Google Scholar]
[141] Kostoff RN, Heroux P, Aschner M, Tsatsakis A. Adverse Health Effects of 5G Mobile Networking Technology Under Real-life Conditions. Toxicol Lett. 2020;323:35–40. [PubMed] [Google Scholar]
